August 19, 2024
Your support has been like a breath of fresh air to anesthesiologists who intubate patients at St. Boniface Hospital and train medical students in the delicate technique.
Thanks to you, St. B was able to order three more C-MAC high-definition video laryngoscopes and monitors this spring, adding to the current fleet of only six such devices at St. B. The new devices arrived in July and were immediately put to good use.
“We would like to thank you and shake your hand.”
The six C-MAC devices St. B had were needed in 14 operating rooms, plus three more rooms in Labour and Delivery, and for offsite needs. There are not always enough C-MACs to meet the demand each day, explained Bruce Knoll, Anesthesia Technologist of seven years at the Hospital.
“That is why the acquisition of these C-MACs was huge for our department,” he said. He mentioned that the budget for replacement parts is limited, let alone for new equipment, making donor support even more important.
“To the donors, we would like to thank you and shake your hand. That’s the importance of this, it’s not just something that’s convenient to have. It is lifesaving,” he said.
It takes at least 20 minutes to clean and reprocess a C-MAC before it can be used again, said Dr. Tamara Miller, Site Lead of Anesthesiology at St. B.
“The C-MACs are in constant use,” she said. “Surgeries can be delayed because we are waiting for the equipment to become available. It holds up our day and means cases run late into the evening because we’ve had to wait for equipment,” she said. “It’s not ideal, but it happens.”
Old method more difficult, risky

Dr. Tamara Miller, shown with training dummy, has less than three minutes to intubate a patient before they run out of oxygen.
Any surgical patient having a general anesthetic must be intubated – have a breathing tube attached to a ventilator – because they will stop breathing on their own.
“We have less than three minutes to secure that breathing tube in the patient,” said Dr. Miller. “That is because from the time they stop breathing until the time we get a breathing tube in place; they’re not getting any oxygen. If it runs out, they can get brain damage or die.” Inserting a breathing tube while the patient is awake can be unpleasant for them and is ruled out unless absolutely necessary, she said.
Traditionally, anesthesiologists have intubated patients using direct laryngoscopy, which is the manual method with a standard metal handle and curved “blade” often shown in movies and on television.
This method is still the most common at the Hospital because there are not enough C-MACs to go around. But it is more difficult and can take precious time, she said. “You have to position the patient exactly in such a way that all the angles line up so you can bend down, and you see where their vocal cords are, which are what you need to get past.”
C-MAC “the gold standard”
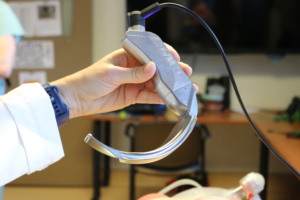
C-MAC video laryngoscope blades have a camera and light at the end, connected to a monitor.
The C-MAC video laryngoscopes are more forgiving. They are equipped with a tiny camera and bright light at the end, giving anesthesiologists a clear view on the monitor screen from inside a patient’s throat.
“These machines really are the gold standard,” said Knoll. “If I was being intubated, I would want to be intubated using one of these. I would feel much safer and be much happier with someone using the C-MAC.”
Added Dr. Miller, “We are securing airways much faster. Because C-MACS have a camera and light and you’re seeing it on the screen, you don’t have to line up all those angles as precisely. You can put the blade in, and you can manipulate it easily to find where the vocal cords are and know where you need to direct the breathing tube.”

Dr. Tamara Miller, Site Lead, and Bruce Knoll, Anesthesia Technologist, are excited about the new C-MACs.
What’s more, video laryngoscopes offer more of a curve. “The beauty of this is, because it’s more curved, it’s a lot easier to get into the airway and see where the vocal cords are,” said Dr. Miller. Standard blades are straighter because our eyesight can’t travel on a curve.
The curved blades also make it easier to train medical students, residents, advanced respiratory therapists, and paramedics to intubate patients. “We do a lot of teaching. With the old method you never had a clue what your learners were seeing,” she explained.
“From a teaching perspective, you have the handle, and your learner is looking down. As their supervisor, you are trying to look over their shoulder to see what they’re seeing. It’s not an easy process to get right,” she said.
“With the video laryngoscopy, you can see exactly where they’re putting it, and you can tell when you need to step in.”




